Aug 18
Navigating the Surrogacy Question
Kilian Melloy READ TIME: 1 MIN. SPONSORED
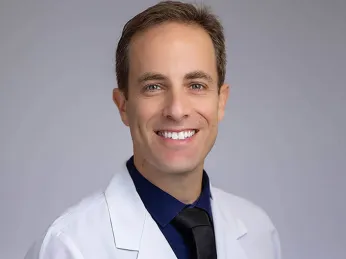
Fertility interventions like IVF have never been more popular among LGBTQ+ couples seeking to welcome genetically related children into their families. The Prelude Network — North America's largest and fastest-growing network of fertility clinics — has made equality central to their foundational philosophy: That everyone who wants to be a parent should have the chance to fulfill that dream.
To this end, Dr. Ido Feferkorn, one of the specialists at The Reproductive Medicine Group in Tampa, Florida, makes working with queer prospective parents a significant part of his practice. This commitment goes beyond words; Dr. Feferkorn demonstrates his dedication through actions like attending the Men Having Babies Conference in Berlin.
Source: Prelude Fertility
To understand fertility treatments, it's essential to know that creating new life requires three biological components: Sperm carrying genetic information from one parent; an egg (ovum) carrying genetic information from the other parent; and a uterus where a fertilized egg can develop and, after nine months of gestation, culminate in childbirth — the arrival of a new individual whose genetic code combines both parents' contributions.
For patients who produce ova and possess viable wombs, completing the combination might be as straightforward as obtaining donor sperm for IUI (intra-uterine insemination), a procedure in which a fertility healthcare provider uses a thin tube to conduct sperm directly into the uterus, where it can more easily reach ova, whose release can be stimulated pharmacologically.
Other patients might need a gestational carrier to provide the womb; they might even need donated gametes (sperm or eggs) as well as a surrogate's womb to complete their family-building journey. In these cases, the gestational carrier typically requires IVF (in vitro fertilization), which involves stimulating the release of donor eggs, then uniting the eggs with sperm under laboratory conditions to create an embryo. After several days, and following genetic testing, the embryo can be implanted into a surrogate's womb.
While each family has unique visions and needs in their quest for parenthood, many families who come to The Prelude Network share a commonality in needing expert facilitation to make successful matches with donors and/or surrogates.
“We do not have our own gestational carriers,” Dr. Feferkorn specifies. “We don't want to be involved in choosing them, just to make sure everything is done completely, ethically right. We give you the list of agencies we work with. The benefit of using agencies on our list is that we know they work according to FDA regulations, with all tests being done and so forth. But even if you decide to work with another agency, we will always make sure that we screen the gestational carriers ourselves, that they meet FDA standards.”

Source: Getty
One of the main points Dr. Feferkorn is sure to highlight is this: "It's not just men who need to use surrogates." People of any gender identity or orientation might need someone else to carry a pregnancy, and the reasons vary widely.
"Obviously, we have same-sex male couples," Dr. Feferkorn explains. "We have single fathers. We have single mothers. We treat anyone who wants to be a parent. If there is no uterus we can use, that can mean the patient’s uterus was removed, or maybe carrying a pregnancy poses a higher risk than is reasonable for the patient."
Regardless of why a surrogate is needed, "We usually recommend creating embryos before we find the gestational carrier," Dr. Feferkorn notes. "The logic is that once we find the gestational carrier we want, they won't necessarily wait until we have the embryos ready. They want to start.”
“You can work in parallel,” Dr, Feferkorn adds, “but we finalize agreements with carriers once we have embryos stored and ready for transfer."
Those agreements are a crucial part of any fertility process involving a gestational carrier, and they’re part and parcel of the work that goes into making the family-building process as successful and stress-free as possible. “There are legal aspects which I'd rather not go into, because I'm not a lawyer,” Dr. Feferkorn says, “but we make sure that both the gestational carrier and the parents have an attorney to make sure that all aspects are covered.” He points out that in some jurisdictions, “you have to actually adopt a child if it's born from a carrier, so we have to make sure that the child does not belong legally to the gestational carrier. In Florida, it's not an issue — but we want to make sure that these legal aspects are taken care of.”
Medical risks, too, are anticipated and avoided as much as is possible. “We make sure that the risks are minimal as can be,” Dr. Feferkorn says. “But sometimes doctors and patients add complications. One common scenario involves the transfer two embryos instead of one in an IVF procedure. The logic is, ‘Okay, I paid so much I want to have two kids out of this.’ Or, ‘We're two dads, and we want to have one baby from his sperm and the other baby from my sperm.’ It all looks fine and dandy when everything goes right. But when we transfer two embryos for a twin pregnancy, the possible complications are vastly greater: Preterm birth, preeclampsia, diabetes — all these complications are more common when you transfer two embryos, and for that reason we will not do it in our clinic.”
“For a couple doing that,” Dr. Feferkorn adds, “they really have to think about what they gain and what they're risking, especially when we have the ability to freeze embryos for years so that we can transfer one now and come back down the road for child number two.” He illustrates his point with the following cost-benefit analysis: “Yes, you may be saving on the gestational carrier by transferring two embryos at once, but you're risking higher costs with prenatal care. You have to make sure that that's balanced out.”

The complexities don’t simply go away if a patient enlists a close friend or family member to serve as a surrogate. “We want to make sure the carrier is doing it out of her own free will and not feeling forced to do it,” Dr. Feferkorn clarifies. “It's wonderful if a sister is happy to help her brother or her sister. But she may feel she has to do it, and that adds complexity to the matter. For that reason, any time we use a gestational carrier there is a psycho-educational consult, and this goes for the couple who will be using the carrier, for the carrier herself, and for all parties together. The purpose of this is a to verify that there’s no pressure to be doing this from the couple or for financial reasons.”
Gestational carriers are typically compensated, of course, but Dr. Feferkorn addresses that point very clearly. “It may seem like that's only about money, that it's only transactional,” he says. “But when you talk to gestational carriers, you find out that, in reality, many of them do it out of altruism. They want to help other couples achieve their family-building goals.
“And many of them do this more than once,” he adds, “and not for financial reasons.” Moreover, he adds, “we have cases where the carrier comes back to help a family with their second and third child. There’s a nice relationship going on. It's beautiful, and we see it quite a lot.”
Dr. Feferkorn points out another aspect: “We also want to provide consultation around the question of how to address the subject afterwards: What do we tell our family? What do we tell our friends? What do we tell a child, and when do we tell the child? All these are important questions, and it's best to address them before we even start the journey.
“We do this whole process hand in hand,” Dr. Feferkorn adds, emphasizing The Prelude Network’s commitment to providing top-quality individualized care to all patients. “It seems overwhelming; you think, ‘Oh my god, I have so many things to do.’ But in the end, it comes down to a checklist. First you do this, and then we'll come to box number two.
“It really is simpler than it seems. I think the hardest thing is finding the right gestational carrier to be a match for you. Some couples’ goal is to have the gestational carrier be part of their life in the future, meaning they want their kids, and themselves, to be in touch with the gestational carrier. Others are more comfortable with having a relationship with the gestational carrier only during the pregnancy and then parting ways. You see all of that, and you want to make sure that your desires are also what the gestational carrier desires. This can take time, and usually finding the carrier is the longest part of the process — it can take eight months to a year to find the right match for you.”
But anything so deeply fulfilling as parenthood is worth taking the time to do right. That commitment to excellence and personalized care comes back to a foundational idea: “Love is love, and family is a family, and from our experiences, the agencies that we work with feel the same,” Dr. Feferkorn sums up. “Many of the LGBTQ community are having their families and are using gestational carriers. It's so common these days that it's not an issue.”
Kilian Melloy serves as EDGE Media Network's Associate Arts Editor and Staff Contributor. His professional memberships include the National Lesbian & Gay Journalists Association, the Boston Online Film Critics Association, The Gay and Lesbian Entertainment Critics Association, and the Boston Theater Critics Association's Elliot Norton Awards Committee.